what does it mean to have arthritis in the spine
Spinal Arthritis (Arthritis in the Dorsum or Neck)
Spinal arthritis is inflammation of the facet joints in the spine or sacroiliac joints between the spine and the pelvis. It may exist related to wearable and tear, autoimmune disorders, infection and other conditions. Sometimes, the inflammation may besides affect the sites where ligaments and tendons attach to the bones of the spine. Regardless of the exact location, arthritis in the back or neck can be painful and ofttimes becomes chronic.
Spinal Arthritis: What Y'all Need to Know
-
Osteoarthritis is the about mutual blazon of arthritis to touch the spine.
-
Arthritis can occur anywhere along the spine, just is more frequent in the lower dorsum and neck.
-
Pain and stiffness are the most common symptoms of spinal arthritis.
-
Causes of spinal arthritis are withal largely unknown except for osteoarthritis, which is typically a consequence of wear and tear.
-
Spinal arthritis treatment may include pain medications, steroid injections, physical therapy and surgery in severe cases.
Spinal Arthritis Causes and Risk Factors
The causes of arthritis in the dorsum or neck vary depending on the blazon of arthritis you have. Besides normal wear and tear and autoimmune triggers, in many cases the exact crusade remains unknown. Genetic components have been identified in connectedness with some forms of spinal arthritis, significant that it may exist hereditary.
Other spinal arthritis risk factors include:
-
Historic period
-
Excess weight/obesity
-
Presence of certain conditions such as diabetes, gout, psoriasis, tuberculosis, irritable bowel syndrome and Lyme disease
Types of Spinal Arthritis
There are more than than 100 different types of arthritis, and most of them may affect the back or neck. Although all arthritis leads to inflammation, arthritis is categorized as inflammatory and noninflammatory (degenerative) based on its origin.
Osteoarthritis of the Spine
Osteoarthritis (noninflammatory or degenerative arthritis) is the most mutual class of spinal arthritis. It usually affects the lower back and develops through wear and tear. Every bit the cartilage between the joints slowly breaks downwardly, it leads to inflammation and pain. Considering the hurting is from mechanical harm, it is typically more noticeable when you bend or twist your back. By back injuries may likewise contribute to the development of degenerative arthritis of the spine.
Osteoarthritis of the spine usually affects the facet joints betwixt the vertebrae. It is also known every bit facet joint arthritis, facet joint syndrome and facet disease. In some cases, degeneration of the spinal discs (degenerative disc disease) may contribute to facet articulation arthritis. As discs between the vertebrae become thinner, more pressure is transferred to the facet joints. This leads to more friction and more impairment to the cartilage.
When these degenerative changes occur in the neck, this condition is called cervical spondylosis. Arthritis in the cervix doesn't always cause pain, and many people have no noticeable symptoms.
Rheumatoid Arthritis of the Spine
Rheumatoid arthritis (RA) is an autoimmune disorder, pregnant that the immune system turns on itself. It attacks synovium — the lining of the joints. Although rheumatoid arthritis is more common in other joints, it can also affect the spine, specifically the cervical region (neck). Rheumatoid arthritis of the spine is not caused by wearable and tear, so it'south considered an inflammatory arthritis. It may crusade back pain (and pain in other joints) even when these joints are non in use. It tends to affect women more than men.
Spondyloarthritis
Spondyloarthritis is a group of inflammatory diseases that affect both the joints and the locations where the ligaments and tendons adhere to the bones (entheses). Spondyloarthritis, although inflammatory past origin, is not the aforementioned as rheumatoid arthritis.
There are several forms of spondyloarthritis — some are more common in the spine than others:
-
Ankylosing spondylitis is a type of spinal arthritis that may crusade inflammation of the vertebrae and the sacroiliac joints at the base of the spine. In severe cases, several vertebrae may fuse together and cause a hunch in the dorsum.
-
Psoriatic arthritis is a condition associated with psoriasis — an autoimmune disorder better known for the itchy, scaly rash. People typically develop psoriasis before arthritis, but sometimes it is reversed. Although more mutual in smaller joints, it may also affect the spine.
-
Reactive arthritis is articulation inflammation triggered by infection somewhere else in the body — oftentimes in the bowel or the genitals. Reactive arthritis in the spine normally occurs in the lower back and tends to go away on its own.
-
Enteropathic arthritis is a grade of arthritis linked to inflammatory bowel disease (IBD). Not all people with IBD develop arthritis, and of those who do, non all go it in the spine. Enteropathic arthritis flare-ups tend to sync with IBD flare-ups, but the timing and intensity may vary from person to person.
-
Other forms of spondyloarthritis include undifferentiated spondyloarthritis (when symptoms don't friction match any of the known types) and juvenile spondyloarthritis (when symptoms begin in babyhood).
Co-ordinate to a different nomenclature, if a particular type of arthritis involves the spine and/or sacroiliac joints, information technology is called axial spondyloarthritis. If other joints and tendons are involved, this is called peripheral spondyloarthritis. Many people experience both types at different points in the progress of their spondyloarthritis.
[[degenerative_spine_conditions]]
What are the symptoms of spinal arthritis?
Symptoms of spinal arthritis may differ from person to person. In general, they may include:
-
Back and neck pain, specially in the lower back
-
Stiffness and loss of flexibility in the spine, such every bit existence unable to straighten your back or turn your cervix
-
Swelling and tenderness over the affected vertebrae
-
Feeling of grinding when moving the spine
-
Hurting, swelling and stiffness in other areas of the body (especially in inflammatory arthritis)
-
Whole-body weakness and fatigue (more common in inflammatory arthritis)
-
Pain and numbness in your arms or legs if the nerves are affected
-
Headaches (in case of arthritis in the neck)
Although back hurting is a mutual symptom, not all people have it, even those with advanced spinal arthritis. On the other paw, some may experience pain even before arthritis can be seen on an X-ray.
In certain types of spondyloarthritis, centre inflammation (iritis or uveitis) may occur, causing pain, watery eyes and blurred vision.
Spinal Arthritis May Contribute to Other Issues in the Spine
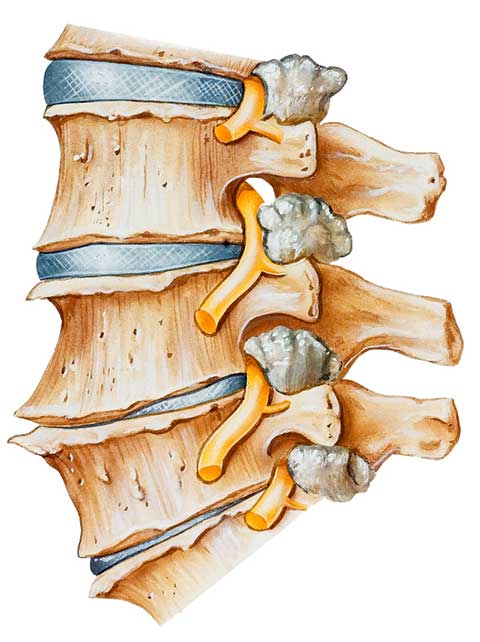
Spinal arthritis may crusade os spurs — overgrowths on the edges of the bones. In the spine, bone spurs particularly impact facet joints, making them abound larger. This condition is called facet joint hypertrophy. Although bone spurs on their own are not harmful, they may narrow the passages for the spinal string and the nerves exiting the spine. This may lead to two painful conditions:
-
Spinal stenosis – compression of the spinal cord inside the spinal culvert
-
Radiculopathy – pinching of the peripheral nerves as they exit the spine (sciatica is one blazon of radiculopathy)
Ankylosing spondylitis (the boring calcification of the ligaments between the vertebrae) may also crusade additional problems such every bit:
-
Stress fractures in places where new bone has formed
-
Collapsed vertebrae
-
A spinal deformity called kyphosis
How is spinal arthritis diagnosed?
Your doctor may employ some or all of the following diagnostic methods to confirm spinal arthritis:
-
Medical history and concrete examination
-
Claret tests for genetic markers and/or RA antibodies
-
X-rays of the spine to locate the arthritic articulation
-
MRI, CT scan, myelography, bone scan and/or ultrasound to zero in on the damage, discover nerve and spinal string interest or dominion out other causes
-
Joint aspiration: testing of the synovial fluid inside a joint
To pinpoint the painful joint, your dr. may numb information technology with an injection and check whether the pain goes away.
How is spinal arthritis treated?
The handling for spinal arthritis depends on many factors. They may include your age, level of pain, blazon and severity of arthritis and personal health goals. Because the joint damage caused past arthritis is irreversible, the treatment usually focuses on managing hurting and preventing further damage.
Nonsurgical treatments for spinal arthritis may include:
-
Nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids (pills or injections) to reduce hurting and swelling
-
Other medications targeting specific symptoms or triggers of inflammatory arthritis
-
Physical therapy to improve dorsum muscle strength and range of movement in the spine
-
Lifestyle changes to reduce inflammation or stress on your spine: losing weight, quitting smoking, changing your posture, etc.
Surgery for Spinal Arthritis
Surgery may be recommended for spinal arthritis if other treatments don't sufficiently relieve pain. The goals of the surgery may include:
-
Decompressing the spinal cord and freeing upward the nerve roots from os spurs and other tissues that may be pressing on them
-
Stabilizing the spine by fusing several segments together in a procedure chosen spinal fusion
These surgeries tin can be performed every bit open procedures or with a minimally invasive arroyo. There are pros and cons to each method. The surgeon will review and discuss the options before the operation.
Source: https://www.hopkinsmedicine.org/health/conditions-and-diseases/spinal-arthritis#:~:text=Spinal%20arthritis%20is%20inflammation%20of,disorders%2C%20infection%20and%20other%20conditions.
0 Response to "what does it mean to have arthritis in the spine"
Post a Comment